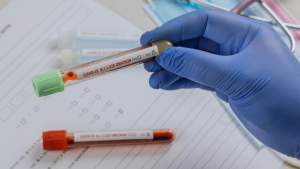
It was in early March 2020 when the first media reported, Covid-19 course in women and men. "That is why Corona meets men stronger," was the headlines, or "the small difference: why the new coronavirus is particularly dangerous for men". According to statistics, the articles refer to interesting figures: According to statistics, at that time, women fall more often to Covid-19, but men are more likely to die from it-in certain age groups with almost 50 percent increased risk. In the meantime, the number of infections are almost balanced. What remains: Men have to go to the intensive care unit much more often than women because of a corona infection.
Christine Hidas, senior physician in charge of the Central Emergency Department at Darmstadt Hospital, can confirm this: "We have definitely admitted more men than women. Even middle-aged men are more severely ill than women with Covid, were more often hospitalized and were more likely to be in intensive care." More often than women, the Darmstadt doctors had to connect their male patients to the ECMO, a device used in acute respiratory failure.
If you are looking for the reasons for the differences, you come across various explanations: According to studies, women develop especially before the menopause when they are at work - because they work more than men in professions where the risk of infection is high on the basis of many contacts: In nursing or retail, for example. "No home office is possible, these women still had to go to work in the Lockdown," explains Ute Seeland, specialist in internal medicine and deputy chairwoman of the German Society for Gender Medicine. "Perhaps they used the tram to get to work and brought the children to kindergarten beforehand."
Zealand has a second explanation for why women are now more likely to contract Covid-19, even though they take the pandemic more seriously than men on average and adhere more strictly to distancing and hygiene rules. It lies at the molecular biological level: "The genetic code for ACE-2, a protein that plays a key role in infection and is, so to speak, the entry point, lies on the X chromosome. And women have two of them." The doctor suspects that more ACE-2 is available in the body of women, which makes it easier for the virus to penetrate cells.
Why there is still a difficult course and death due to Covid-19 is less common than in men is due to the hormones: estrogen circulates in the blood of women. "The sex hormone inhibits the cytokine storm," explains gender doctor Seeland. This is an overreaction of the immune system, for which the body produces plenty of cytokines such as interleukin-6 in the late stage of the disease. They fuel the defense so much that this phase of the disease hardly deals with the virus: The extreme activity of the immune system is then the real danger and can cause a life -threatening multi -organ failure.
Long Covid is more common in women than in men.
According to Ute Seeland, the immune system of women is more flexible than that of men, but thanks to the estrogen better in balance. “The men don't get staggered so quickly. But if so, it is difficult to regulate again. For me, this explains their increased mortality from Covid-19. «The doctor published a study with colleagues for whom the team examined the positive influence of estrogen on the course of the disease. The group came to the conclusion that therapy with sex hormones could improve the survival rate of women who are seriously suffering from covid if they already have the menopause behind them and therefore no longer have their own estrogen.
It is now clear that women are more often affected by Long Covid than men. The immune system reacts to Sars-CoV-2 similar to a rheumatic disease, which often affects women, suspects senior physician Hidas. "It's as if their immune system just can't rest. But this could also be due to the fact that women were already exhausted before the infection, because they had twice the burden of homeschooling the children."
Women and men react differently not only when they have Covid-19, but also when they get a vaccination against it: in February 2021, the US Centers for Disease Control and Prevention published data according to which three quarters of the vaccine side effects affect women. If there is an allergic shock after vaccination, then almost never in men. "It's the same as always," says Hidas, who is also the chairwoman of the Frankfurt Group of the German Medical Association. "Active ingredients are only tested on men, and if you then treat all of them, new side effects come out in women.«
Her colleague Seeland is convinced that half or a third of the usual vaccine dose against Covid-19 would be sufficient for women. "Women should not get the same amount as men. It's nothing new that they respond more strongly to vaccinations because their immune system is more active." The fact that the dose-finding curves are not at least adjusted to the body mass index (BMI) annoys the doctor: "We haven't learned anything, everyone just carries on as before."
Consider gender differences to comprehend infections
As before, this has meant for decades: Women either do not receive any attention in medical studies or the scientists do not evaluate the data separately according to gender – which, in view of the physical differences, would not only make sense, but would even be urgently needed. "Mixing the data of both sexes distorts the result immensely," says Hidas. "But in Germany, unlike in Austria, for example, it is not mandatory. As far as gender medicine is concerned, we are the deepest province."
The data from Sabine Oertelt-Prigione proves that there is still a lot of room for improvement. The professor of gender-sensitive medicine at the universities in Bielefeld and Dutch Nijmegen has examined more than 4,400 scientific studies on Covid-19 with researchers from the Netherlands and Denmark. In the specialist magazine »Nature Communications«, the team published the terrifying results of its meta -analysis: The evaluation was separated from gender in only four percent of the studies.
Yentl disorder
The importance of gender medicine is well known. Already 30 years ago, Bernadine Healy, an American cardiologist, lamented the unequal treatment of men and women in medicine. In the editorial of the "New England Journal of Medicine" in 1991, she lamented the "Yentl syndrome" - in reference to the novella "Yentle, the Yeshiva Boy" by Isaac Bashevis Singer.
The story of the Nobel Prize for Literature is about the Jewish girl Yentl, who disguises himself as a man to study at a religious school. Healy also said that cardiac patients should best dress up as men in order to be well cared for medically. Otherwise they would have to prove to be as heart -sick as a man to experience the same treatment. Statistics agree with the now deceased cardiologist: Studies show that women die more often after a heart attack than men. And that their chances of survival rise when a doctor treats her.
Oertelt-Prigione considers this to be alarming: "From the beginning, we were able to see that this disease progresses differently in women and men. This is indicated by the numbers of hospital admissions and deaths. Drugs and non-pharmacological measures could therefore have different effects depending on whether the patients are female or male."
First of all, the professor suspected that the problem was due to the time pressure at the beginning of pandemic. The first author, Emer Brady from Danish Aarhus, commented on this in a press release from the university: »In terms of time pressure, we hoped that the progression of pandemic would grow awareness of how gender and gender are related to the disease. “It was assumed that increasingly more study protocols will be registered with the focus of gender and gender. "Unfortunately that was not the case."
This is not only dangerous, but a missed opportunity, says Oertelt-Prigione: "Taking a look at gender differences has often helped to better understand the infection in Covid. It will also help us improve medical treatment. Taking gender differences into account is an essential step towards personalized medicine."
"Corona has boosted interest in gender-sensitive medication."
In a way, the pandemic was a kind of stroke of luck for her field, says gender physician Seeland, who is involved in the Margarete Ammon Foundation for the promotion of gender-specific medical research: "Corona has given gender-sensitive medicine a boost and exposed the weaknesses of the health system, such as understaffing and underpayment in care." If it were up to Zealand, gender medicine would be a medical subject in its own right, "like anatomy or cardiology".
Germany, however, is still a few changes from this: So far there are only two institutes, one at the Berlin Charité, the other at the University of Bielefeld. "22 percent of the universities have gender-sensitive medicine in the form of lectures and seminars in the curriculum, they are my hopes of hope," reports Seeland, but also demands examination relevance: "Only what is checked is learned." In addition, textbooks have to be written and elearning Offer formats, because so far there is only very little teaching material.
If you ask Zealand when the ignorance of women in medicine began, the doctor says: "With the witch hunt. If women in the Middle Ages were familiar with medicine and healing, they were burned. From then on, the doctrine was purely male, the women were considered weak, sick and suffering. Only 20 years ago, the medical society in the United States confessed that women are not little men."
The pandemic would have clearly shown that not everyone should be treated equally, says Hidas from the Medical Association. “So we could have thought of gender medicine from the start. Now we have loud data worldwide that have not been evaluated gender. One would have to ask Mr. Lauterbach if he could do it afterwards. ”Hidas comes from Hungary, all women in their family were employed. The lack of equality in her professional branch sometimes stunned her, says the doctor: "Medicine is an old men's club."
Will gender medicine ever be taken for granted? "Only if it had an economic advantage," says Hidas. "If anyone proved that you can save money by treating men and women with Covid differently, I am convinced that something would change."
Gender medicine is not about creating a new medicine for women and keeping the existing one for men. "Unlike some believe, gender -sensitive medicine is not women's medicine," emphasizes doctor Seeland, "because she does not exclude the men." Rather, it is about spreading knowledge that there are differences between men and women. Medicine will improve this at least in the future - for everyone.
Studies involving female mice and men
Take height, muscle mass, hormone influence, kidney function, metabolism, immune system - male and female body differ. Sometimes they sometimes use drugs. Nevertheless, science often does not separate between men and women in the development of new medication. This starts with animal experiments that are preceded by studies with people: in eight out of ten departments, researchers mainly examine male animals.
In 1977, the U.S. Food and Drug Administration (FDA) even banned women of childbearing potential from enrolling in Phase I and early Phase II trials so as not to put pregnant women at risk. The knowledge gained by the men was simply transferred to female patients. With sometimes fatal consequences:
Since 1993, pharmaceutical companies in the United States have been asked to include both genders in their attempts. However, this only makes sense if the data is also evaluated gender -separated - otherwise the results appear distorted. In Germany, however, only twelve percent of the admission studies for cardiac medication represent the side effects gender -specific. All others show data for the entire group of subjects - although women develop more side effects than men.
In Germany, "in the sum of all phase I studies for a drug, a proportion of women of 10 to 40 percent," reported the "research-based pharmaceutical companies" in May 2021. These are studies in which the "behavior" of the new active ingredient in the body is first examined, "without the influence of hormone fluctuations or hormonal contraceptives". This is most likely to be realized with men. In phase II and phase III studies with patients, the proportion of women is then 30 to 80 percent.
On January 31, 2022, Regulation No. 536/2014 adopted eight years earlier comes into force to the European Union (EU), which is supposed to correct the grievance. According to this, all participants in a clinical examination should be representative of the population groups - this includes age and gender. Exceptions are possible, but must be well founded. The regulation applies to all clinical exams carried out in the EU, but not to non -interventional studies.