In 1924, the bacterium Streptococcus mutans was first associated with caries. The English dentist James Kilian Clarke found the microorganism in a tooth hole and declared it the culprit. Since the bacterium was easy to cultivate and study outside the mouth, scientists collected more and more evidence in the coming decades that seemingly substantiated the guilty verdict: S. mutans is adept at attaching itself to hard tooth surfaces, it loves the sugar in food and produces acid. It thrives best in an acidic environment that eats holes in the enamel. In the 1960s, many dentists considered S. mutans to be the cause of caries, in the mid-1970s, scientists even developed a caries vaccine from whole bacterial cells. The researchers did not yet suspect that the vaccine was directed against the wrong thing. Because later it turned out that S. mutans was not solely responsible for the tooth damage, but received support from other microbes.
It has been known for centuries that microorganisms live in the mouth. In the late 16th century, Antonie van Leeuwenhoek reported that he had scratched living bacteria from the inside of his mouth and that it "moved very nicely" under one of the microscopes at that time. Later scientists cultivated everything they could find in the mouth and analyzed the properties of the bacteria. They tried to attribute diseases to certain microbes. With the modern sequencing techniques that have established themselves in the past two decades, as well as new imaging procedures, researchers are now available to completely different options. You can determine which microbes are in the mouth, how they are structured and which functions you fulfill. As a result, the long -cherished views are changing about how the oral microbioma contributes to dental health - and also to general health. This could open up new ways to use the microbial community in terms of health.
Series: Mouth-friendly
Whether talking, eating, smiling or kissing: our mouth is almost constantly in motion. However, many people only notice how important it is that he stays healthy when the first aches and pains become noticeable, such as caries, gingivitis or nasty canker sores. Oral and dental care can have far–reaching consequences for the entire body - it is now even associated with diseases such as Alzheimer's, heart disease and Covid-19. You can find out what optimal oral hygiene looks like, what contribution the oral microbiome makes and what makes the oral mucosa so special in our series "Healthy in the mouth":
The microbiome of each mouth corner is unique.
Members of the community remain constant, even though new microbes regularly enter the mouth when eating, breathing, or biting nails. But not all survive in the oral cavity. On average, a person is home to around 250 species there, about 700 potential mouth dwellers are known. These species can evade the antimicrobial defense of saliva and are adapted to life in a warm, humid environment that is regularly oxygenated.
On closer examination, however, it turns out that the oral microbiome is not a homogeneous collection of living beings, but rather an assortment of different mini-microbiomes located in different regions of the mouth. The microbes seem to be specialists in the niche they each occupy. This applies to the most frequently examined areas such as saliva or dental plaque as well as to the tongue, cheeks, palate, throat or tonsils.
"Places in the mouth that are only a few millimeters away are inhabited by completely different microbial communities," says Jessica Mark Welch, microbe researcher at the Marine Biological Laboratory in Woods Hole. She and her colleagues wondered how the bacteria ended up in the individual niches and how they manage to survive there: »We wanted to understand how the bacteria work together. To do this, we had to examine the overall structure. "
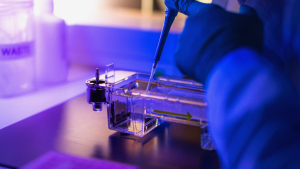
Mark Welch's colleague Gary Borisy, a cell biologist and imaging specialist who now works at the Forsyth Institute in Cambridge, helped develop a new microscopy method. With the help of fluorescence, 15 or more bacterial species can be imaged simultaneously. Using this technique, Borisy and Mark Welch examined dental plaque, a biofilm consisting of microorganisms that are stored together. In this case, the microbes had organized themselves in a hedgehog-like arrangement. Thread-like bacteria piled up on top of each other, forming a spiny main structure. Other organisms had nested between the spines. The whole thing happened in a healthy mouth. However, other studies have shown that the species composition and the physical structure of the biofilm change when someone gets sick.
During her training as a dentist in the early 1990s, she was taught that biofilms are always bad in the mouth, says Egija Zaura, an expert in microbial ecology in Amsterdam. This view has since changed. It seems to depend on which microbes the biofilm contains. Since it has been clearly proven that regular tooth brushing promotes dental health, the associated removal of biofilms should therefore have an overall positive effect on the oral microbiome, says Zaura. At least in people who consume a lot of starch and sugar. The long-term stability of the community suggests that health-promoting microbes that were present in a biofilm grow back after brushing their teeth and protect the teeth from the next acid bath. A study has also shown that people with periodontitis, a bacterial inflammation of the dental bed, develop a new, more species-rich biofilm after a professional dental cleaning.
How bacteria enhance oral health
It is now clear that in a healthy mouth the entire microbial community works together and thus does its service to the human host. Some roommates, for example, Streptococcus salivarius, have an anti-inflammatory effect. In addition, the oral microbiome contributes to the regulation of acidity. Caries-free people have species in their mouths that are able to convert arginine or urea from food into pH-neutralizing ammonia. Other metabolic products of the bacterial community help to kill pathogens.
The microbes based there not only support oral health. They transform the nitrate that we absorb over fruit and vegetables into nitrite, which in turn is converted into nitrogen monoxide. The fabric helps to regulate blood pressure. Like many other mammals, humans have apparently outsourced the task of nitrite production to the microbes living in the mouth in the course of their development. Alex Mira, bacterial geneticist at the Fisabio research institute in Valencia in Spanish, says: »Our body does not have the necessary enzymes for this. We rely entirely on our oral microbiome. "
Free -selling, antiseptic mouthwashes can destroy useful microbes in the mouth and disturb this important process. In contrast to toothpaste, many mouthwashes contain the active ingredient chlorhexidine that kills the microbes directly. As Mira reports, ten years ago in dentistry there was an opinion that the oral cavity must be kept clean and eliminated as many oral bacteria as possible. This is considered wrong today. A study from 2020 has shown that the saliva microbioma of healthy people who washed their mouth with chlorhexidine solutions changed significantly. The acidity in her mouth increased that her body was less nitrite available, and they tended to a higher blood pressure.
A repository for oral microorganisms
Until recently, dentists blamed dental health problems on various microbes: S. mutans was supposed to be responsible for caries, Porphyromonas gingivalis for periodontitis, and Candida albicans was suspected of causing oral candidiasis, better known as oral thrush.
"In dental diseases, we were very influenced by the idea that every illness has a single, microbial pathogen," says Mira. In the late 1990s, researchers began to change their views. Scientists from the Forsyth Institute suspect, accumulation of organisms below the gumsum could be responsible for dental disorders. Floyd Dewhirst, dentist, pharmacologist and microbiologist at the Forsyth Institute, deals with periodontitis. He was one of the first to recognize the importance of the microbial communities in the mouth-long before cost-effective DNA sequencing techniques were available.
In the early 2000s, as modern sequencing techniques became increasingly available, Dewhirst recognized an obstacle to progress in this field: Although researchers could distinguish them based on their unique genetic sequences (they studied the 16S rRNA), they were unable to name the different oral bacteria or understand their relationships to other microbes. Dewhirst therefore set about developing a comprehensive database and a preliminary naming system. This spawned an important resource for the field: the Human Oral Microbiome Database.
The work of Dewhirst and others made it possible to catalog the entire spectrum of microbes known today at different sites in the mouth. This was done as part of the Human Microbiome Project, one of the world's first large-scale studies of the microbiome of healthy people. During the project, samples were taken from nine sites of the oral cavity. The composition of the bacterial community differed so much from person to person that it was impossible to identify features for a healthy microbiome. However, the combinations of those microbes that prevailed in a particular place were similar. Less dominant species, on the other hand, were very different individually.
Uncontrolled microbiome
The data from the Human Microbiome Project confirmed that there are potential pathogens in the mouth in both healthy and sick people. Not only S. mutans, but also other acid-producing bacteria such as bifidobacteria or lactobacilli have sometimes been associated with oral diseases. Later research confirmed that – depending on the person - different microbial profiles may be associated with caries.
The latest theories assume that a change in the microbial community in the mouth means that species that are normally kept in chess by other microbes and cause mund diseases. "These bacteria are kept under control in a healthy ecosystem," says Mira. "They multiply, change their gene expression and become pathogens." He and others postulate that mouth diseases have a polympical origin. In his opinion, the reason that the efforts to make a caries vaccine have so far been in vain is that the candidates are only directed against a single microbe that may not be involved.
Another mystery that could be solved with more knowledge about microbial communities in the mouth is the following: Why do only a fraction of people with mild gingivitis develop periodontal disease? It could be that the mere presence of a biofilm is less important than its exact composition. People who actually develop gum disease appear to have microbes in their mouths that, as the disease progresses, interact differently with the immune system and trigger more tissue-destroying inflammation. Microbes that thrive in this environment prosper – a vicious circle develops: disturbances of the ecosystem and inflammation fuel each other.
Considering oral bacteria and their host as part of the same ecosystem gives a more complete picture of what determines a person's dental health. Does she often eat sweets? How often do your teeth come into contact with fluoride through toothpaste or drinking water? Such factors can put pressure on the microbial community, trimming it towards health or illness. In other words: the lifestyle is important, but you can not control everything with it.
A treasure trove for biomarkers
In the event of more and more diseases - including colon cancer, rheumatoid arthritis and Alzheimer's - researchers observe a changed composition of the oral microbiome.
Whether there is a causal relationship here can probably only be clarified in a few years. In the meantime, scientists are investigating whether changes in the oral microbiome could reliably indicate that a particular disease is developing or progressing. In the search for biomarkers, the oral microbiome is of particular interest because it is easily accessible and easy to handle. Compared to the gut microbiome, the influence of diet also seems to be minimal. The stability of the microbial community in the mouth therefore offers great potential for biomarkers.
With the help of one of the world's largest supercomputers, a team from the Oak Ridge National Laboratory (ORNL) in Tennessee is processing huge amounts of data. They contain information about the microbiome of various parts of the body, including the mouth. The researchers are looking for patterns that could lead them to medically relevant biomarkers that indicate neurological diseases such as Parkinson's, Alzheimer's and amyotrophic lateral sclerosis (ALS). "There are microbes that are found in periodontitis and Alzheimer's. Perhaps we will also find a connection between Parkinson's and ALS, " says Joseph Chris Ellis, microbiologist and bioinformatician at ORNL. One of the goals is to find indicators that indicate early on that someone has an increased risk of illness. "Maybe then we will be able to develop new drugs with which we can prevent or treat the onset of these diseases.«
Manipulation of the microbiome specifically
The mainstays of today's dentistry are operations and antibiotic treatments. But research on the oral microbiome could usher in an era in which the microbes in the mouth are precisely manipulated. In order to promote dental health, it may even be possible to specifically add certain strains to the oral microbiome.
The goal is to detect aggressive strains in a person's mouth and replace them with others in order to fine-tune the bacterial community, says Mark Welch. The currently available probiotics are probably not up to this task, because the microbiome in the mouth hardly allows for changes. "It's not easy to integrate a foreign bacterium into the oral community," says Dewhirst. Because it does not fit into the network of organisms that are picked out in the course of life, because they harmonize particularly well.
Mira's working group has identified a candidate for an oral probiotic: Streptococcus Dentisani. This bacterium, which isolated the researchers from caries -free people, helps to kill pathogens in the mouth. The nickname Dentisani comes from Latin and means healthy teeth. The team is currently dealing with how this extremely demanding bacterium can give people. At the same time, the researchers try to overcome the regulatory hurdles for the market launch of a probiotic.
Another approach could be to chemically alter the oral environment to prevent tooth decay and other diseases. Toothpaste with ammonia-producing, pH-lowering arginine is already on the market. Prebiotics could come next, Mira speculates. For example, nitrate could be added to toothpaste, either as a salt or as a plant extract, in order to specifically feed certain bacteria and thus promote health.
The regular visit to the dentist could also serve to pursue more targeted prevention strategies, says Zaura. It suggests that dentists examine the microbial community of a person as well as the condition of the teeth. In this way, they could recognize weaknesses early and intervene in the microbial ecology of the mouth to avoid oral and possibly other diseases. "If you pay attention to oral health, you can do a lot for general health," says the microbiologist.
This article translated by is part of "Nature Outlook: Oral health", an editorially independent supplement produced with the financial support of third parties.
© Springer Nature Outlook: Oral Health, 10.1038/D41586-02920-W, 2021