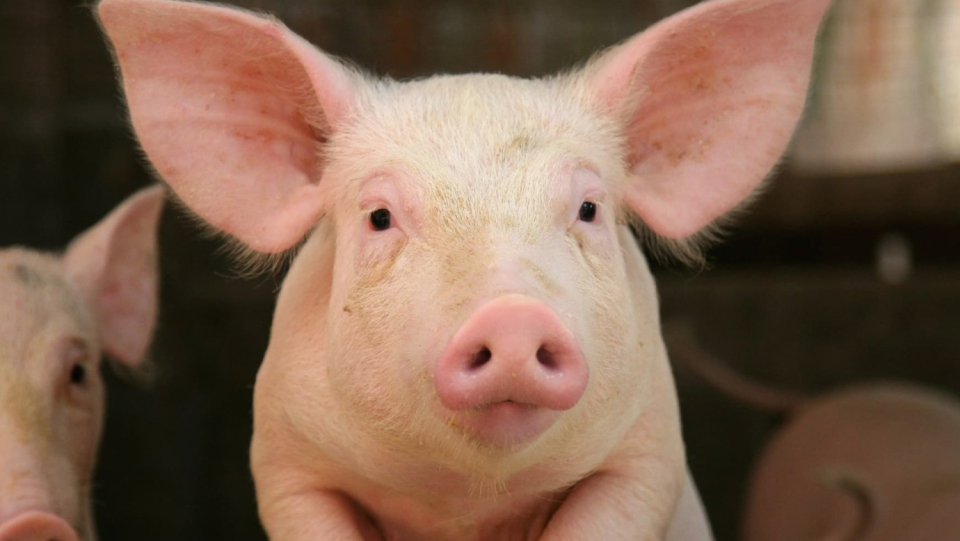
David Bennet's heart failed. The 57-year-old handyman from Maryland had only weeks to live. Since he had disregarded treatment instructions in the past, he was not eligible for a donor heart; at least not for a human one.
At the beginning of January 2022, his doctors offered him to get a pig heart. He accepted the offer. "I know it's a shot in the blue, but it's my only chance," he said, according to a press release from the University of Maryland Medical Centers in Baltimore, in which he was dealt with. On January 7, the doctors transplanted the heart that was genetically changed so that it can be accepted by a human body.
Bennet survived eight weeks with his new heart before his body gave up. After his death, the scientists found that the transplanted organ was infected with a herpes virus typical of pigs, which had remained undetected in the tests.
But a few weeks have been a long time for an animal organ that is used to a person, a procedure called Xeno Transplantation. The human immune system begins to attack pig organs that have not been genetically changed within a few minutes. That is why research colleagues that also deal with Xeno transplantation are impressed by the experiment. "I would never have thought that the patient survived for almost two months," says Luhan Yang, biomedian and managing director of Qihan Biotech in Hangzhou, China. "In my opinion, it is a success for the research field."
This case was just one example of several xenotransplants that made the news this year. A few months after Bennet's procedure, two research groups independently reported that they had transplanted the first pig kidneys into three different people. The persons had been legally declared dead because they no longer had brain function. The series of experiments showed that even two to three days after the procedure, the organs produced urine and were not rejected by the human immune system. In June and July, surgeons performed two more transplants of pig hearts on brain-dead individuals.
Many scientists expect that these early experiments will increasingly lead to small clinical trials in which xenotransplantations are performed on extremely sick people. Proponents emphasize that such attempts – if successful – could ultimately help to significantly shorten the lists of many thousands of people waiting for a donor organ, many of whom will die during the waiting period. Currently, the researchers say that they are waiting for the competent authorities, such as the US Food and Drug Administration (FDA), to review some submitted applications. A spokesperson for the FDA reports that the authority is commenting on the existence or status of such a submission.
Statistics for organ donation
In June, the authority held a session to deal with the growing number of American research teams who officially want to start clinical studies with Xeno transplants. The scientists tried to convince the responsible persons in the authority that the Xeno transplantation was ready for use in humans. For this purpose, they presented data that came from hundreds of baboons that had survived up to three years after a transplant of pig organs - especially hearts, kidneys and insulin -producing island cells.
Clinical trials are needed, the researchers say, to figure out what type of pig is best used and how to make sure the animals don't carry pathogens. "I think we should take this step and do clinical trials," says Wayne Hawthorne, a transplant surgeon from the University of Sydney in Australia.
Bennet's transplant and subsequent death brought unprecedented attention to the issue – but also highlighted the risks. Scientists are well aware that they need to proceed with caution. "If a bigger problem arises, it could set back the entire field of research," warns Hawthorne.
Animal donor
Xenotransplantation has long been a dream of transplant physicians, who have always been struggling with a lack of suitable organs. In the 1960s, researchers began transplanting chimpanzee and baboon organs into humans with limited success. The rearing of so many animals turned out to be impractical.
Pigs turned out to be more sensible donors because they are closer to people in size and anatomy and are already raised in large quantities in agriculture. In some respects, pig organs could even have some advantages over human donor organs. Operations could be set in the presence and the organs are transplanted in a fresh state instead of the patient and medical team at all times in the event that a genetically suitable donor dies.
In addition, doctors do not always know the medical history and genetic predispositions of a human donor. "When we check donors, it takes an hour, we don't have more time," says Jay Fishman, a infectious disease specialist at Massachusetts General Hospital in Boston. In pigs, he says, "we can do tests that we can't use in humans."
Until the early 1990s there was a big problem with pig organs: the human immune system was picked up. The Transplant Surgeon David Cooper from Massachusett's General Hospital found a solution. He discovered that the immune system of humans and other primates react primarily to a sugar molecule on the surface of the pig cells, namely to α-gal. If you now change the pork regenery that encodes the protein that this sugar molecule also produces, you prevent the cells from producing α-gal. Organs that come from the changed animals could survive much longer in non -human primates.
The development of so-called gene editing using CRISPR-Cas9 in the 2010s proved to be a catalyst for research. It not only simplified the modification of the gene involved in the production of α-gal, but also a number of other genes that make it easier for the human body to accept the pig organs. Several companies are now developing pig organs with various modifications; so far, none of these have been released for clinical trials beyond the limited trials to date.
Those pigs used in Bennet's transplant came from the Revivicor company in Blacksburg, Virginia, and had ten genetic changes. The company changed four pig genes, including one that allows the pig to grow organs at the size suitable for humans. In addition, they added six human genes: four that suppress the immune response, and two that prevent the blood from clotting as a result of inflammation.
The approaches of other teams differ from this approach. Makana Therapeutics, who are based in Miami, have only modified three genes of the pigs. The changes in these genes prevent human antibodies from attacking the organ and most of all seem to improve the chances of survival of the organs in non -human primates, says company founder Joe Tector. "The better the genetic engineering gets, the easier it will be to add or replace DNA," he explains.
Eckhard Wolf, a molecular biologist at the Ludwig-Maximilians-University in Munich, agrees. "Our basic strategy is to keep everything as simple as possible," he says. His team has made five genetic changes in a wild breed of dwarf pigs. The first offspring were born in September. These dwarf pigs do not require any change in terms of the size of the organs, as they are naturally similar to those of humans. If everything goes well with the planned transplantation of the mini pig organs into baboons, Wolf says, the European Medicines Agency (EMA), which regulates the approval of medicines and medical supplies in the EU, could agree to a small human study with such hearts within the next three years.
More data is required
Since the first human studies have only just begun, every genetic modification was initially tested exclusively on non–human primates - although some species tend to develop more antibodies against pig organs than humans for reasons unknown so far. It is still unclear which, or even if any of the changes will be relevant for transplants in humans.
Despite the differences, some research teams say that they were stopped by the FDA to provide more data on how well pig organs work in non -human primates. "It is like saying that everything indicates that an active ingredient works differently in humans than in monkeys - but still let us test it on monkeys," says Cooper. "It is completely illogical to do that." The FDA did not comment on how much data from experiments with primates need in individual cases. However, she published a guideline in which it is said that the studies on primates are not sufficient to be able to ensure that pig organs are harmless to humans.
Transplantations in brain -dead people could represent an intermediate step. The surgeon Robert Montgomery from New York University, who heads a team that has transplanted a kidney this year, is planning further transplants in brain dead before applying for clinical studies with living individuals. The Revivicor pigs, which he had used in his experiment, showed only a single genetic change that dealt with α-gal; With this genetic modification in December 2020, the FDA released pigs for consumption and for some medical applications, which did not include transplants. Montgomery fears that a complex combination of several genetic changes could have unpredictable interactions.
Other researchers think that studies on living people are the best way to find out if the body still rejects transplants months after the procedure. Keeping brain-dead people alive for so long could be unethical, says Jayme Locke, a transplant surgeon at the University of Alabama at Birmingham. She led another team that transplanted a kidney into a brain-dead person. Locke is working to get permission from the FDA to conduct clinical trials with kidneys from the same Revivicor pigs that were used for Bennett's heart. Her team has already applied for such a study in the nationwide register, but it has not yet been released, and they have not even started to determine the 20 patients who could receive the kidneys.
Other fabrics, such as the insulin -producing island cells, could hardly trigger any immune response at all, which is why a group of easier genetic changes could possibly be sufficient, says Hawthorne. His team bred a number of pigs for the production of isolated cells that have no α-gal and have two additional genes that are supposed to dampen the human immune reaction. In June 2022, his team reported that the transplanted island cells had healed five paves of diabetes. The animals lived over two years without having used insulin or immunosuppressive medication.
Hawthorne is now planning a clinical trial in which the islet cells from pigs will be used in people suffering from a severe form of type 1 diabetes, which causes blood sugar to drop extremely quickly. Should his team find the financial support, he says, the trials could begin within the next year – provided they are given free rein. Other research groups have previously found that pig islet cells appear to be harmless to humans.
Disease -resistant pigs
One of the biggest concerns of the authorities with regard to the new technologies is the possibility that the pigs could have communicable diseases. It is not clear how big this problem actually is, but diseases could become a problem in several ways. Pathogens that affect pigs could pass from the transplanted organs to humans. This concern led Qihan Biotech to slow down its efforts in the field of xenotransplantation when African swine fever broke out in China earlier this year. This development led Yang and her colleagues to biotechnologically develop a pig that is resistant to this disease. The manuscript in which you present your work is currently being reviewed.
In addition, there are endogenous retroviruses (Porcine endogenous retrovirus = PERV), viral elements that occur in the genetic material of the pigs. These are not absorbed from the surrounding area, but are parts of innate viral DNA. They are harmless for pigs, but according to the study situation, it is unsure whether they can pass from an organ into human cells and thus be dangerous for humans. "It is still too early to find out whether this is a real danger or just a hypothetical one," says Yang.
To see if it is possible to inactivate these viral elements, Yang and George Church at Harvard Medical School in Boston used the gene scissors CRISPR to mess up the bases of all known PERVs in the pig genome, thus disabling the PERVs. There were a total of 62 changes in the cells of the pig kidneys, a record value in gene editing.
"There were a lot of doubts about whether you can make so many changes and still produce viable donors," says Michael Curtis, managing director of the biotechnology company eGenesis in Cambridge, Massachusetts. Church and Yang founded eGenesis to bring the CRISPR technology for xenotransplantations to market maturity. One of her macaques with a transplanted kidney from a pig with dozens of PERVs turned off survived for almost a year. The company is now using its technology to make pork hearts, kidneys and livers, which have up to 80 changes, depending on the purpose.
But even if you get rid of the PERVS and protect yourself against all known pathogens, one cannot prevent an unknown virus from doing damage, says Fishman. "There are still undiscovered pathogens that could come from pigs," he explains. For example, a person with an xenot -transplanted lung could get a respiratory disease that otherwise only affects pigs.
Fishman says it's unlikely, but viruses that infect two different species could recombine in the human body. This could lead to a new pathogen, just as influenza viruses do in birds, bats and pigs. To keep the risk to the public low, the FDA recommends transplanting porcine organs only into people who have no other choice and whose quality of life could be significantly improved by the procedure. The agency says it has strict guidelines for long-term monitoring of patients because of the risk of disease transmission and prohibits people with pig organs from donating blood.
Bennet's heart turned out to be harboring porcine cytomegaloviruses (CMV), which belong to the herpes virus family and often infect pigs. However, it is still unclear whether it was they who cost Bennet his life. Muhammad Mohiuddin of the University of Maryland Medical Center led the study that accompanied Bennett's surgery. He says there is no evidence that the virus has damaged the heart. He is also sure that the virus has not spread to the rest of Bennet's body. He suspects that the patient's organs have already been damaged by his illness or the complications after the procedure – regardless of the swine virus. Nevertheless, Mohiuddin cannot rule out that the virus played a role in all of this. Revivicor had tested his pigs for RNA from CMV, together with other pathogens, and had assured that they were healthy. Mohiuddin and others suspect that the virus was latent in the organ and could have been detected only by antibody tests in the animal. Revivicor says that they have developed more sensitive CMV tests, but did not answer the question about the number of pathogens they are testing for.
Mohiuddin, whose team was given permission to carry out bennets transplantation, plans to carry out further such interventions as soon as he can be sure that the future donor organs are free of viruses. He says that the treatment centers repeatedly offer him patients who would be good candidates and willing to receive a pig organ, but so far he rejects them. "Before I can satisfy someone differently, I have to be satisfied myself," he notes.
Pork livers for dialysis
Even if the first xenotransplantation of a heart attracted a lot of attention, the first organ that will reach study maturity will probably be the kidney, says Tector. This is because it has a simpler structure than most other organs. As for more complex organs, eGenesis is planning an intermediate step. They hope to start testing pig livers in an arrangement reminiscent of dialysis in the next 12 to 18 months. Three to six participants who are close to death would be individually connected to one pork liver each. Your blood will be passed through the organ to filter out those toxins that accumulate in liver failure. Curtis says that the company is also working on young pig hearts, which could similarly serve as a transition for children with heart problems until they get a human donor heart.
At their hearing in June, the responsible people of the FDA presented a list of concerns about Xeno transplants, among which, among other things, the quality aspect of the organs and the question of how to make sure that they are free of pathogenic. "There are many questions we have to answer," says Tector. However, he says that 60 to 70 percent of Makana's Paviane survived with a functioning pigeonator for more than a year and that the company was therefore ready for clinical studies. Therefore, they have already submitted the corresponding application.
When the studies actually start, says Fishman, it will be the most important thing to collect as much data as possible from every subject. "We owe this to the patient and society."
© Springer Natur BegrenzTnatur, 10.1038/d41586-022-03794-2 , 2022