Many medicines that take women during their pregnancy were hardly researched. In an interview, Georg Schmidt explains why this is the case and why vaccination against the Covid 19 virus is an exception. He is a cardiologist and chairman of the working group of medical ethics commissions in Germany.
"Do not take this medication if you are pregnant or breastfeeding." Such a sentence is often read on package inserts. Why is so little known about the effects of drugs on pregnant women?
Georg Schmidt: In clinical research, pregnant women are among the particularly protective - vulnerable - people such as children and adolescents. In order to research the effect of a medication or a vaccination, valid reasons are needed.
Why are expectant mothers particularly vulnerable?
Pregnant women are not alone. They carry an unborn thing. And this has to be protected. The consequences of medicines for the development of the embryo are actually difficult or not predicted. From an ethical point of view, we pregnant women can only include in medication studies if you or your child could benefit personally. If this direct expected benefit is missing, we leave pregnant women alone.
When is this the case?
An interesting example is vaccination against Covid-19. From studies, we know that pregnant women who are infected with the Covid 19 virus have a three- to five-fold risk of increased risk of a severe course. Among other things, this is probably due to the fact that your immune system changes during pregnancy. The cells of the embryo represent a foreign body, so to such a way. So that the immune system does not reduce it, the immune system is driven down. This is important for a successful pregnancy - for women itself, however, it means a tendency to get a higher risk of developing a virus disease or other infections. There are also considerable physical changes.
Which ones, for example?
The volume that the heart pumps in a minute increases almost half during pregnancy. So the heart has to do significantly more during pregnancy. The larger the child becomes, the more space it takes. In the last trimester, it usually presses on the inner organs.
Pregnant women can therefore no longer breathe so deeply ...
Exactly, your respiratory volume decreases, the heart rate continues to increase. In this situation, a serious infection is a huge additional burden on the body. There is a lack of capacities, the body can reach its limit. In addition, there are changes in blood clotting, which increase the tendency to blood clots and embolism.
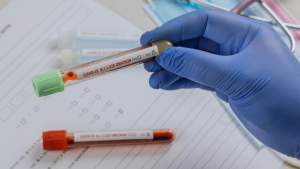
Corona vaccination advice for expectant or nursing mothers, as well as women who want to have children
Pregnant and breastfeeding women are called upon to be vaccinated against the coronavirus, because the vaccination protects mother and child. The Standing Committee on Vaccination (STIKO) recommends primary vaccination with two doses of the Covid-19 mRNA vaccine Comirnaty (BioNTech/ Pfizer). "Pregnant women, regardless of their age, should be vaccinated with Comirnaty and not with Spikevax," it continues. If the pregnancy had been detected after the first vaccination had already taken place, the second vaccination should only be carried out from the 2nd trimester.
In contrast, the STIKO recommends a Covid 19 vaccination with two doses of an MRNA vaccine at a distance of 3 to 6 (Comirnaty) or 4 to 6 weeks (Spikevax). Still end under the age of 30 should be vaccinated with Comirnaty.
For women of childbearing age, especially those who wish to have children, the STIKO expressly recommends the Covid-19 vaccination "in order to be optimally protected against this disease in a future pregnancy from conception over the pregnancy".
Further information on corona vaccination can be found on the pages of the Robert Koch Institute.
So the corona vaccination would give pregnant women a decisive advantage and justify testing the vaccine clinically on them?
It's not that easy. Only because the women would draw a potential benefit from the vaccination at this point does not mean that we now approved a randomized, double -blind clinical study. We have to weigh up all known and possible risks against the expected benefit - for the pregnant woman and the unborn. And because this is affected with so many uncertainties, we try to gain as much information as possible from other sources. The study itself is actually the last step and we slowly get on these keys.
That is?
We collect and analyze all available data. Like every new drug, vaccines are first tested on animals, even on pregnant animals. In addition, the data comes from studies with non -pregnant women. In addition, information about the course of pregnancy and the development of the child of pregnant women is collected, which were given a vaccination outside of a clinical examination for whatever reason.
Even if the Covid-19 vaccine is a good example of when pregnant women are included in clinical research, the problem remains that many drugs women take during pregnancy have not yet been tested on them. How is it known that many of the drugs that pregnant women take do not harm either mother or child?
Here we draw out of experience. By that I mean data from women who, despite their pregnancy, have taken an approved medication for various reasons. If problems arise, you will be reported to the Federal Institute for Medicines and Medical Devices. This procedure is called pharmacovigilance system. The meaningfulness is of course not nearly as large as with a planned controlled study, but it provides valuable information over the years. For example, medication such as paracetamol or ibuprofen has been taken by pregnant women for decades. Based on the reports received, there is, for example, the recommendation not to take ibuprofen in the last third of the pregnancy, as the child can lead to heart and kidney problems.
What to take into account when studying pregnant women
The chairman of the working group of medical ethics commissions, Georg Schmidt, considers it to be justifiable under certain circumstances to carry out a study with pregnant women. This would be the case, for example, if a clear medical benefit for the pregnant woman or the child can be expected. This can also be the case if a dramatic hazard of the pregnant women and/or the child are revealed in the context of a pandemic. Here, waiting for results from observations of pregnant women outside of studies can take too long.
It is always important that the scientific methods, i.e. the study design, are suitable for answering the question.
Could it also be that some side effects show up so late that they are no longer associated with taking medication during pregnancy?
There is no complete security. Whenever possible, women should do without taking medication during pregnancy. This "possible", of course, includes that funds are sometimes necessary. Then the benefit is higher than the risk and taking medication. We have to live with this uncertainty and weighing up.
What about Zika? An infection with the mosquito-borne virus is particularly dangerous for unborn babies, as has been known for five years now. Why is there neither a Zika vaccination nor a drug prophylaxis so far? Shouldn't clinical trials with pregnant women be booming here?
It is true: In a Zika infection, studies indicate that the virus can transfer to the unborn child and lead to malformations of the brain. Other neurological abnormalities are also associated with the infection. In this case, expectant mothers are particularly at risk. But in Asia alone, epidemiological data indicate widespread use. No acute outbreak areas are currently known worldwide, the risk is low. Medicine tests on pregnant women are not justifiable from an ethical point of view.
Ebola, on the other hand, remains a threat. The last outbreak in Congo, for example, was only a few months ago. In the meantime, there is a vaccination. However, this is not recommended for pregnant women. They have a particularly high risk of dying from the infection. They can also transmit the virus to the newborn during birth via the amniotic fluid. So why is the vaccine not yet being tested on expectant mothers?
Here, too, we have to collect data first. According to the European Medicinal Medicines Agency (EMA), there are, for example, around 300 reports from women who vaccinated with Ervebo during pregnancy or were pregnant shortly after vaccination. Severe unwanted side effects do not seem to have existed here. However, this small number of cases is not sufficient for a general recommendation. But if a pregnant woman has a clear risk of infecting herself with Ebola. Then the potential benefit predominates and according to EMA, vaccination is appropriate. The data of these cases will be collected and evaluated accordingly in order to adapt the recommendations in the future.
Can't a clinical trial replace that?
No. To vaccinate an expectant mother who does not have a special risk remains ethically unacceptable. Therefore, I would not support a vaccination study specifically on pregnant women at this time.
How can it be prevented that something like that does not happen again as in the case of the sedative Contergan? The drug resulted in severe malformations in unborn people (see info box).
It is terrible what happened then. However, a repetition is no longer conceivable. In fact, the incident has led to the development of the global drug safety standards that we have today, and that we are so cautious about pregnant women.
What went wrong at that time with Contergan?
In Germany, the calming and sleeping pills of Thalidomide (Contergan) was approved without a prescription on October 1, 1957. It had a calming effect, remained unobtrusive in animal experiments and showed no questionable side effects during the first applications in humans. The manufacturer recommended the drug, among other things, in the event of nervousness, fears and sleep disorders as well as against pregnancy. With devastating consequences: The remedy was only apparently free of side effects. In fact, it damaged the nerves and influenced the development of the embryo. Depending on the time of pregnancy the medication was taken, it disrupted the formation of extremities, skull or internal organs. A total of around 5,000 children with countergan damage were born in Germany. There was also an unknown number of dead births. The Contergan scandal gave the reason for the adoption of the German Medicines Act, which now sets the standard for drug safety in Germany. The process against the manufacturer was discontinued in December 1970 with a comparison.