In Germany, about 9000 people need a vital donor organ, almost 300 of them need a lung. On average, they wait one to two years for these. This is also due to the fact that only 40 to 50 percent of potential donor lungs can be transplanted – for example, because their blood types must also match the recipients. Canadian researchers from the Toronto General Hospital Research Institute have now developed a method with which they can change the blood type of lungs. This is reported by Aizhou Wang's team in the journal Science Translational Medicine. Treatment with certain enzymes changes the blood type from A to 0. Organs with this blood type are compatible with all other blood types and can therefore be donated to more people.
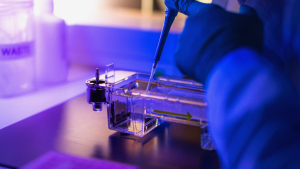
The scientists carried out the method of eight lungs that could not be transplanted. To do this, connect the organs to a device that supplies the tissue outside the body with liquid-a process that is referred to as ex-vivo-lung perfusion. They added two enzymes to the circulating solution. Within four hours, almost all antigens of blood group A were removed from the cells of the lungs, so that they ultimately had blood group 0. Then they tested whether antibodies against the A-antigen caused a rejection reaction. None of the organs reacted to what confirmed the success of the enzyme treatment.
A lung treated in this way is particularly suitable for recipients with blood group 0. Antibodies circulate in their blood that would immediately attack and destroy donor organs of the more common blood groups A and B. As a result, they wait longer on average for a suitable organ and have a 20 percent higher risk of dying before a suitable donor is found.
It is unclear whether the treated lungs will form their original blood group A again over time, and if so, when: the enzymes that assemble the antigen of blood group A continue to circulate in the tissue. Whether this would have health consequences, however, is not said: kidneys, for example, can be transplanted with certain precautions, although the blood groups of the recipient and donor are not compatible. Here, too, antibodies against the transplanted tissue are formed over time without rejection.