Just two years ago, Sars-CoV-2 began its triumphal march around the globe. Today, the highly contagious Omyron variant is driving incidences to record highs. Meanwhile, doctors have a growing arsenal of therapies available to keep the disease at bay. But their limited availability and complicated logistics make it difficult for medical professionals to decide who should receive the drugs. Below you will find an overview of the therapies available to patients in the hospital and at home.
Therapies for non-hospitalized patients
Monoclonal antibodies: In freshly diagnosed patients with a high risk of severe covid 19 processes, the recommended therapy usually consists of monoclonal antibodies-proteins produced in the laboratory that bind to the Coronavirus and prevent body cells infested. Administered within ten days of the diagnosis (intravenously or under the skin), the artificial antibodies reduce the proportion of hospital stays and deaths by more than 80 percent.
The new Okron variant, however, carries mutations in the part of its genome targeted by monoclonal antibodies. "There is currently only one antibody that works," says Michelle Barron, a professor of medicine at the University of Colorado School of Medicine and medical director of infection prevention and control at the nonprofit health system UCHealth. The active ingredient called sotrovimab from GlaxoSmithKline and Vir Biotechnology can only be administered intravenously.
"From a logistical point of view, this is something completely different from a syringe in the leg or in the arm," says Barron. "You have to set aside at least an hour for the infusion and be healthy enough to make it to the place of treatment." For providers of therapy, this also raises the question of where to carry it out. "Of course, you don't want sick people to walk through a full waiting room.«
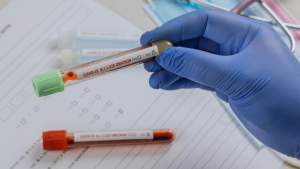
Antiviral pills: Last month, the US drug authority FDA approved the emergency use of two antiviral drugs that can be taken as tablets at home: Paxlovid from Pfizer and Molnupiravir from Merck and Ridback Biotherapeutics. Paxlovid's examination is still running in the EU. However, the Federal Government has already ordered a million packs of the medication to be delivered during the year.
In studies on adult high-risk patients, Paxlovid, taken within ten days of symptom onset, was able to reduce the risk of hospitalization and death by 89 percent, molnupiravir by 30 percent. However, Paxlovid also has its risks: for example, it consists of a combination of the antiviral drugs nirmatrelvir and ritonavir. "Ritonavir is an old HIV drug that is known to interact with all sorts of things," Barron says. "So many high-risk patients may already be taking a drug that interacts." Therefore, before a pharmacist issues a prescription, he must check all the patient's other medications.
Access: However, the biggest challenge for most outpatient treatments is the scarce offer. In Germany, the monoclonal antibody Sotrovimab has not yet been not available. In the United States, the active ingredient was still available directly from wholesalers last autumn. This relieves the procurement easier and medical facilities. However, when the use of monoclonal antibodies increased sharply due to the beginning of the omicron wave, the US Ministry of Health began to monitor the distribution to the states and territories. Since then, each state has received a limited ration that is based on the incidence and hospital stays. According to the federal guidelines, the states are now primarily intended to give the funds with the highest risk of serious illness. And since Sotrovimab is the only monoclonal antibody that works well against omikron, demand is high.
With antiviral drugs, the availability does not look much better. They should also be used primarily for outpatients with the highest risk. "Yesterday, our health care system issued the first dose of Paxlovid — to one person," David Boulware, a physician and infectiologist at the University of Minnesota School of Medicine, said in an interview with Scientific American Jan. 7. As of January 10, Zuckerberg San Francisco General Hospital and Trauma Center has received just 20 packs of Paxlovid," said Monica Gandhi, an HIV and infectious disease physician at the University of California, San Francisco. The clinic treats 100,000 patients annually and takes over 20 percent of the city's inpatient care."
New York City with its population of more than eight million and more than 30,000 infections a day received around 1,600 doses of Paxlovid in the first week of January, says Celine Gooper, doctor and expert for infectious diseases at New York University Grossman School of Medicine. The reason: The US Health Ministry distribute the pills per capita and not on the basis of the infection rates.
For every patient who comes to the antiviral pills, many immunocompromised high-risk patients go away empty-handed. "They ask me: You don't have this, you don't have this, what do you recommend now?" says Boulware. For such cases, Boulware suggests considering the antidepressant fluvoxamine or the cortisone preparation budesonide – these low-cost drugs, which are also available in Germany, have shown some benefit in initial clinical trials on non-hospitalized Covid patients.
Repurposed medications: Fluvoxamine can inhibit those inflammatory reactions that are typically associated with severe Covid-19. In a randomized study with 1497 outpatient Covid high-risk patients in Brazil, there were about 90 percent fewer deaths among those who had received a ten-day treatment with fluvoxamine. Also, the need for emergency care in this group decreased by 65 percent, compared with patients who received placebo pills at random.
Budesonide, a steroid for inhaling, is usually used to prevent asthma symptoms. In a large, open study in Great Britain, in which older, non -hospitalized patients with comorbidities such as high blood pressure and diabetes took part, the medication showed slight advantages. For those who began using the inhalator within two weeks of the occurrence of the Covid symptoms, the duration of the symptoms decreased by about three days. "So there is a small benefit, especially in the second week of illness," says Boulware.
Treatments for hospitalized patients
For hospitalized Covid patients whose blood oxygen levels have dropped so much that monitoring is necessary, the National Institutes of Health recommend the widely available and relatively inexpensive steroid dexamethasone. It can be taken in tablet form or intravenously. Remdesivir, an intravenously administered antiviral drug, is also offered to hospitalized patients with a severe inflammatory reaction – and often simultaneously with dexamethasone. "It's better to give remdesivir earlier," says Boulware. "If you are in the intensive care unit for the first time and are being ventilated, the benefit is less.«
In order to prevent Covid-19 from worsening to this stage, the US health authority NiH recommends that in its guidelines updated this month in some patients also high doses of intravenous heparin, a medication to prevent blood clots. "It is new to the fact that heparin in therapeutic dosage is now recommended for patients before they come to the intensive care unit," says Farid Jalali, gastroenterologist in Laguna Hills, California, whose theories about covid-lung injuries were published in the blog for emergency medicine Rebel em.
Also, some arthritis medications such as baricitinib or tocilizumab can be given to hospitalized Covid patients from two years of age to dampen inflammation in severe illness. Baricitinib is taken as a tablet, tocilizumab is administered as a drip through the vein.
The future of "old" cancer treatments
Recent research results suggest that Remdesivir could also be helpful for outpatient covid patients. A randomized study, which appeared in December in the "New England Journal of Medicine" in December, shows that covid -related hospital stays and deaths under 279 symptomatic, non -hospitalized patients who received remdesivir were 87 percent lower than in 283 patients in the placebo group. "It looks really good and the supply is not a problem," says Barron. However, she realizes that "logistics is a small challenge because the infusions take three days."
Similar logistical hurdles and ambiguous study results, on the other hand, have cast doubt on the usefulness of the once eagerly studied blood plasma of recovered Covid patients. "Plasma has fallen somewhat into disrepute," says Barron. However, new research could revive interest. On 21 December, the results of an unreviewed study were published. According to the study, the number of hospitalizations among 1181 patients decreased by 54 percent when such convalescent plasma was administered within the first eight days after the onset of Covid symptoms.
"We've all learned that you have to be flexible," says Barron. "What is considered the best therapy can change quickly, you just have to cope with it.«
© Springer Nature Limited Scientific American, THESE ARE THE LATEST COVID Treatments, 2022